FOR HEALTHCARE
PROFESSIONALS ONLY
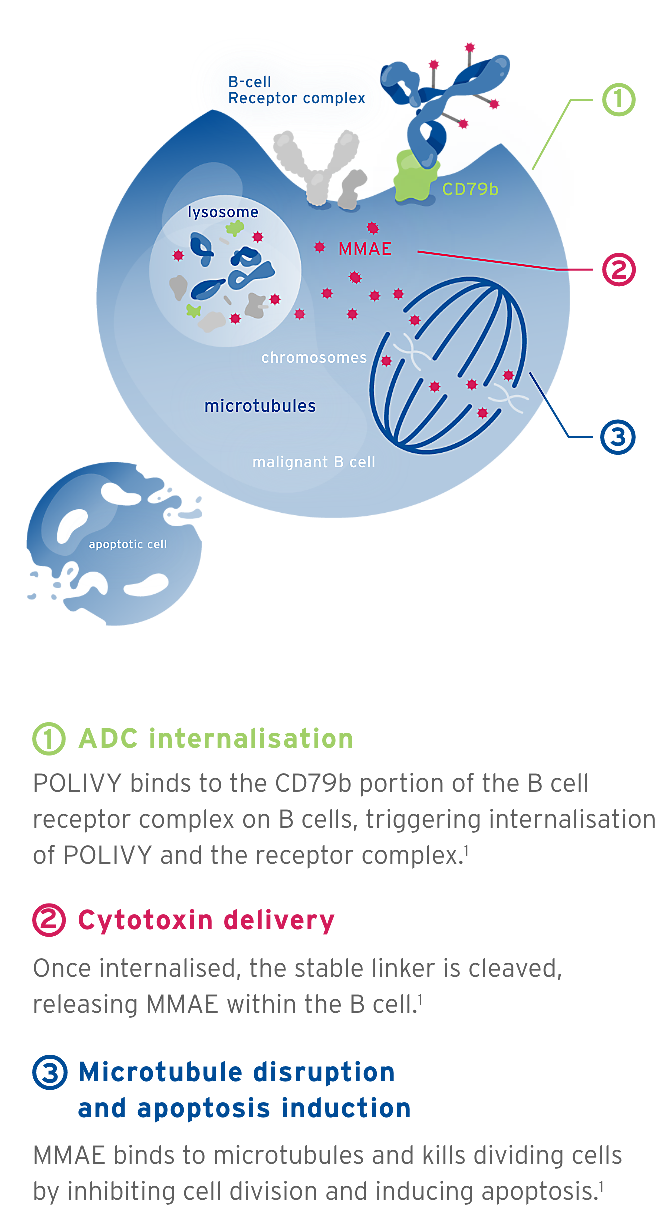
This website is a global information resource. It is intended for healthcare professionals outside of the United States of America (US) who are interested in information on POLIVY®. This website is not country-specific and therefore may contain information which is not applicable to your country. Please refer to your local Prescribing Information for full details.
If you are a US healthcare professional, click here